
Menu
close

The term “transgender” refers to when an individual’s gender identity does not align with the sex assigned to them at birth. “Transgender” embodies a personal and social identity that diverges from societal or cultural norms related to gender, leading to a pursuit of alignment through various means. Learn about the potential side effects of transgender hormone therapy during MTF transition and how to manage them for a safer and successful journey.Some focus on personal expression and social recognition, while others opt for medical intervention, such as transgender hormone therapy.
Transgender hormone therapy is a medical treatment designed to align an individual’s physical characteristics with their gender identity. This therapy involves administering hormones not produced in adequate amounts by the individual’s body, with the type and dosage depending on their specific needs and goals.
For male-to-female (MTF) transitions, feminizing hormone therapy includes medications to reduce testosterone levels and estrogen to promote female secondary sex characteristics. The process of transgender hormone therapy begins with an evaluation by a healthcare professional who specializes in transgender care. Once deemed appropriate for hormone therapy, the healthcare professional develops a personalized treatment plan.
MTF transitions through transgender hormone therapy can have various side effects, both desirable and undesirable. Awareness will help individuals anticipate and prepare for these changes.
The reduction in testosterone levels naturally leads to a diminished sex drive. This change can affect sexual relationships and personal satisfaction. Moreover, lower testosterone levels contribute to fewer erections and a decrease in the volume of ejaculation. Generally, the impact on libido, erections, and ejaculation can vary widely among individuals.
Testicular atrophy — the medical term for the shrinking of the testicles — is a permanent change and often aligns with the desired outcomes of those seeking a physical transition. Testicular atrophy usually leads to reduced sperm production, which explains the decreased ejaculation volume mentioned above.
Breast development is a desired and affirming change, usually beginning a few months after starting hormone therapy. The extent of breast growth varies significantly among individuals, influenced by genetics, age, and hormone dosage.
The reduction in testosterone — particularly its derivative dihydrotestosterone (DHT) linked to male pattern baldness — can slow down or stop the progression of scalp hair loss. This physical change can improve a trans woman’s self-esteem.
The reduction of testosterone levels also plays a crucial role in minimizing the density, coarseness, and rate of hair growth in areas typically associated with male patterns, such as the face, chest, and back. This change results in a more traditionally feminine appearance.
Testosterone is also vital in maintaining and building muscle bulk, so decreased levels of this hormone also mean reduced muscle mass and strength. These changes reflect the body’s adaptation to a more traditionally feminine physique.
MTF transgender hormone therapy makes the redistribution of body fat follow a more traditionally feminine pattern, accumulating around the hips, thighs, and buttocks rather than around the abdomen. This shift contributes to a more feminine silhouette, reflecting the body’s response to the hormonal changes.
Transgender hormone therapy is undeniably transformative and empowering, but the treatment requires careful professional healthcare oversight. The physical side effects — intertwined with mental health considerations — highlight the importance of a supportive and knowledgeable healthcare provider.
HEALOR recognizes the complexity of this journey, offering specialized transgender hormone therapy services guided by compassion and medical expertise. We commit to supporting you in achieving a body that reflects your true self, with the utmost care for your overall health.
Call us at (702) 362-2273 or contact us online, and let us talk about your transition goals.

Discover the positive impact of estrogen therapy in HIV positive transgender women. Is it Safe for HIV Positive Transgender Women to be on Estrogen therapy? Learn about the benefits and considerations for hormonal therapy in this insightful blog post.
Transgender women who are HIV positive often face unique challenges and considerations when it comes to their healthcare. One area of concern is the use of hormone therapy, specifically estrogen therapy, which is commonly used for gender affirming purposes. This article aims to explore the safety of estrogen therapy for HIV positive transgender women. We will examine the existing research and guidelines on this topic, addressing potential drug interactions, side effects, and the overall impact on HIV management.
HIV screening and prevention are crucial for all individuals, including transgender women. According to national guidelines, all transgender persons should be screened for HIV at least once. Repeat screenings should be based on an individual's risk assessment. Understanding the sexual history of transgender women is essential for effective risk assessment, including questions about both receptive and insertive intercourse. Prevention strategies, such as condom use, may be challenging for transgender women taking feminizing hormones, and alternative options should be explored.
Pre-exposure prophylaxis (PrEP) is a biomedical intervention that involves taking antiretroviral medication to prevent HIV acquisition. Studies have shown that daily oral PrEP with tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC) can effectively reduce the risk of sexual HIV acquisition in various populations. While limited data is available specifically for transgender women, a sub-analysis of a large trial suggests that PrEP can be effective when taken as prescribed. However, adherence is crucial, as individuals who seroconverted had no detectable levels of TDF in their blood. Transgender women should be educated about the importance of PrEP and any potential drug interactions with their hormone therapy.
Non-occupational post-exposure prophylaxis (nPEP) is another prevention strategy that involves taking antiretroviral medication after potential exposure to HIV. The guidelines for nPEP in transgender people are similar to those for non-transgender individuals. However, social marketing and awareness campaigns should be tailored to transgender populations to increase awareness and accessibility.
Hormone therapy for transgender women, including the use of estrogen, is not a contraindication for HIV treatment. In fact, providing hormone therapy in the context of HIV care may improve engagement, adherence, and viral load suppression. The World Health Organization and the U.S. Department of Health and Human Services recommend antiretroviral therapy for all individuals living with HIV, regardless of viral load or CD4 count. While there are potential drug-drug interactions between estrogen and certain ART agents, most ART can be safely used with estrogen. Exceptions include Amprenavir and unboosted fosamprenavir, which are not recommended for co-administration with estrogens although the data against these exceptions is not very strong however is best to avoid.
Estrogens are metabolized by the cytochrome P450 enzyme system, which can interact with ART agents. However, data on drug interactions between hormones and ART in the context of transgender care are limited. It is important to monitor estrogen levels and consider adjustments in hormone therapy or ART if necessary. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), ritonavir-boosted protease inhibitors (PIs), or cobicistat with integrase strand inhibitors (INSTIs) may affect blood levels of hormonal contraceptive agents. Transgender women should be informed about potential interactions and encouraged to report any symptoms or side effects.
Transgender women with HIV may require treatment or prophylaxis for opportunistic infections. It is essential to consider potential drug interactions when prescribing medications such as Trimethoprim-Sulfamethoxazole (TMP-SMX). There have been reports of hyperkalemia when spironolactone, commonly used in hormone therapy, is combined with TMP-SMX. Close monitoring of electrolytes and renal function is recommended when these medications are used together.
In conclusion, estrogen therapy for HIV positive transgender women can be safely integrated into their overall HIV management. It is crucial for healthcare providers to screen for HIV, assess risk, and provide appropriate prevention strategies tailored to transgender individuals. PrEP and nPEP can be effective in reducing the risk of HIV acquisition in this population. When it comes to hormone therapy, careful consideration of potential drug interactions and monitoring of hormone levels is necessary. Overall, a comprehensive and individualized approach to healthcare for HIV positive transgender women is essential to ensure their well-being and quality of life.

Article Written by: Cynthia Garcia
In a world that's increasingly acknowledging the diverse needs of its citizens, health insurance is no exception. The LGBTQ community, historically marginalized and often overlooked, has unique healthcare needs that demand specialized attention. Is Your Health Insurance LGBTQ Inclusive? Read on
Whether it's ensuring coverage for gender-affirming treatments or addressing specific health disparities, choosing the right insurance policy is pivotal. But how do you discern if your health insurance truly understands and caters to the complexities of LGBTQ health?
Join us as we delve into the intricacies of LGBTQ-inclusive health insurance and why it matters more than you might think.
Securing proper healthcare, while crucial for everyone, carries added weight for the LGBTQ community. Discrimination, stigma, and inadequate knowledge among medical professionals have historically made healthcare access challenging for many within the LGBTQ umbrella.
While everyone is at risk for common ailments, certain health issues, such as HIV/AIDS, are more prevalent within the LGBTQ community. Moreover, transgender individuals may require treatments like hormone therapy or surgeries that are essential for their well-being.
More so, due to societal pressures, discrimination, and other unique stressors, LGBTQ individuals tend to experience higher rates of mental health disorders like depression and anxiety. Proper coverage ensures access to necessary therapy and counseling services.
Lastly, regular health screenings, like mammograms or prostate exams, should be accessible regardless of one's gender identity or expression. An inclusive policy recognizes and facilitates this need.
Historically, the LGBTQ community has faced significant barriers in accessing quality healthcare. Whether it's been denial of care, substandard treatment, or outright discrimination, these experiences underscore the importance of having inclusive policies in place.
One of the foundations of effective healthcare is trust. Many LGBTQ individuals have faced traumatic experiences in medical settings, making it crucial for insurance providers to prioritize policies that will help rebuild this trust. This can be achieved by guaranteeing access to LGBTQ-friendly professionals and services.
Without adequate coverage, many vital services, from gender-affirming treatments to mental health therapies, can be prohibitively expensive. Inclusive health insurance ensures these costs don't deter individuals from seeking necessary care.
Navigating the maze of health insurance policies can be daunting. Yet, for the LGBTQ community, the stakes are even higher. It's not just about finding a policy with the lowest premiums or the most comprehensive coverage—it's about finding one that recognizes and addresses their unique needs. So, what should one look for in a genuinely inclusive health insurance plan?
At the foundation of any genuinely inclusive health insurance policy should be a clear and robust non-discrimination clause. This policy ensures that individuals are not denied coverage or services based on their sexual orientation, gender identity, or gender expression.
One example of an insurance policy that does not discriminate is Medicare. The federal health insurance program, primarily for seniors, has taken strides to ensure its policies are inclusive and non-discriminatory. For those who depend on Medicare but notice gaps in coverage, it might be beneficial to explore and compare Medigap quotes. In a nutshell, Medigap is a supplemental insurance policy designed to cover the "gaps" or out-of-pocket costs not covered by Original Medicare, such as copayments, coinsurance, and deductibles, ensuring beneficiaries have more comprehensive health coverage.
Central to many transgender and gender non-conforming individuals is the ability to access gender-affirming care. This includes hormone therapy, surgeries, and other related medical interventions. An LGBTQ-inclusive insurance policy should cover these treatments, recognizing their importance in the overall mental and physical well-being of the individual. Such coverage not only ensures that these treatments are financially accessible but also signifies a broader acceptance and understanding of the transgender experience.
Given the unique societal pressures and potential for discrimination, many LGBTQ individuals face an increased risk of mental health challenges. Inclusive insurance policies must offer comprehensive mental health support. This involves coverage for counseling and therapy and ensures access to therapists familiar with LGBTQ-specific issues, enabling individuals to receive the nuanced care they require.
Having coverage is one thing, but having access to LGBTQ-friendly and knowledgeable medical providers is equally crucial. An inclusive health insurance plan should have a diverse provider network, including professionals who are not only accepting of LGBTQ patients but are also trained in their specific health needs.
Despite the strides made in healthcare inclusivity, barriers persist that may hinder LGBTQ individuals from accessing truly inclusive health insurance. Identifying these obstacles and finding ways to navigate them can make the path to comprehensive coverage smoother.
One of the primary barriers is a simple lack of awareness. Many within the LGBTQ community may not be aware of the specific health benefits they should be looking for. Educational outreach through community programs and online resources can bridge this knowledge gap. Partnerships with LGBTQ advocacy groups can facilitate workshops and seminars highlighting the unique healthcare needs and the importance of tailored insurance.
For some, especially those who are underemployed or face economic hardships, the cost of health insurance, even if inclusive, can be prohibitive. Exploring public health options and subsidies can offer some relief. Community health centers and local LGBTQ organizations might also have information on affordable healthcare programs or partnerships with insurance providers offering discounted rates.
Living in areas where LGBTQ acceptance is still a work in progress can pose challenges in finding LGBTQ-friendly providers and inclusive health insurance plans. Telehealth and online consultation services can be a boon in such scenarios. It's also beneficial to connect with national and regional LGBTQ health networks that can guide individuals to accessible resources.
Healthcare is a fundamental right, transcending boundaries of gender, sexuality, and identity. As society moves towards greater inclusivity, our health insurance systems must reflect this progression. By prioritizing genuine understanding, respect, and tailored solutions, we can ensure that everyone feels seen, cared for, and protected in their pursuit of well-being. It's not just about policies or coverage—it's about a collective commitment to a healthier, more equitable future for all.

Discover the significance of differentiating between true gender vs preferred gender in society. Gain insight and understanding on this crucial topic.In a world that is increasingly recognizing the importance of gender diversity and inclusivity, the language we use plays a crucial role in shaping attitudes and perceptions. While the term “preferred gender” has been used in the past to describe a person’s self-identified gender, we argue that the term “true gender” is a more accurate, respectful, and inclusive way to refer to an individual’s gender identity.
To shed more light on the topic, this article will explore the many reasons why “true gender” is the better terminology over “preferred gender.”
The term “true gender” emphasizes the significance of self-identification. It recognizes that an individual’s gender identity is an integral part of who they are, and it is not a mere preference or choice.
Using “preferred gender” can inadvertently suggest that gender identity is a whim or a passing preference, which dismisses the lived experiences and emotions of transgender and gender-nonconforming individuals. By using “true gender,” we honor and validate the authenticity of each person’s self-identification.
Language holds immense power in shaping social attitudes. When we use the term “preferred gender,” it implies that an option or a choice is being made. This language can reinforce harmful stereotypes and discrimination against transgender and gender-diverse individuals, suggesting that their gender identities are less valid than cisgender identities. On the other hand, “true gender” affirms that everyone’s gender identity is equally valid, reducing the potential for stigmatization and discrimination.
Another reason why choosing to use “true gender” is a better option is that it demonstrates respect for each person’s gender identity journey. It conveys the message that their gender identity is real and deserves recognition, regardless of whether or not it aligns with the sex they were assigned at birth. This inclusive language, in turn, promotes dignity and empathy, fostering an environment where individuals can be their authentic selves without fear of judgment or prejudice.
Keep in mind that the language we use can either facilitate or hinder open and productive conversations about gender diversity. “True gender” encourages inclusive conversations by signaling a willingness to engage in a respectful dialogue about gender identity. In contrast, “preferred gender” may unintentionally shut down these conversations by invalidating the experiences and identities of transgender individuals. Choosing the term “true gender” paves the way for greater understanding and acceptance.
Much like with norms and pop culture, language evolves with the times because it reflects societal changes and advancements in understanding.
In recent years, there has been a shift towards using more accurate and respectful terminology when discussing gender identity. “True gender” aligns with contemporary language trends and the principles of inclusivity, making it the logical choice for those who wish to stay current and sensitive to the experiences of transgender and gender-diverse individuals.
Due to the hurdles they’re encountering, transgender and gender-nonconforming individuals often face higher rates of mental health challenges, discrimination, and gender dysphoria. Something as standard as using “true gender” can contribute to a more supportive and affirming environment, which can then have a positive impact on the mental health and well-being of gender-diverse individuals.
Despite being such a small act, using inclusive language in our daily lives is a significant step in fostering a more compassionate society.
Language matters, and the choice between “true gender” and “preferred gender” is not merely a matter of semantics. It reflects our commitment to inclusivity, respect, and empathy toward transgender and gender-diverse individuals.
By embracing “true gender” as the correct terminology, we affirm the dignity and validity of all gender identities, paving the way for a more understanding and inclusive society where everyone can live their truth.

Discover the criteria and clinical process for Diagnosis of Gender Dysphoria. Gain valuable insights and understanding in this comprehensive blog post.
Gender dysphoria is characterized by a marked incongruence between an individual’s experienced or expressed gender and the gender they were assigned at birth. Diagnosis of Gender Dysphoria is a complex process that involves careful assessment by mental health professionals. Let’s explore the criteria used for Diagnosis of Gender Dysphoria, the role of mental health professionals in the diagnostic process, and the steps involved in reaching a diagnosis.
Gender identity refers to an individual’s deeply held sense of gender. It can include identities like male, female, or something unique to the individual. This internal sense of gender is intrinsic and self-defined, not necessarily related to external physical characteristics or societal expectations.
The connection between gender identity and gender dysphoria lies in the incongruence between an individual’s deeply felt gender identity and their assigned gender. When a person’s assigned gender at birth matches their gender identity, they are cisgender. However, for transgender individuals, a discrepancy exists between their experienced or expressed gender and the gender they were assigned at birth.
The old term for gender dysphoria was “gender identity disorder.” However, this term has been retired as it could imply that being transgender is a disorder.
To diagnose gender dysphoria, mental health professionals rely on established criteria outlined in diagnostic manuals such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The same manual suggests that the prevalence of gender dysphoria is within 0.005–0.014% of the population for individuals assigned male at birth and around 0.002–0.003% for those assigned female at birth. The key criteria for diagnosing gender dysphoria are as follows:
Individuals with gender dysphoria typically experience a strong and persistent desire to be of a different gender than the one they were assigned at birth. This desire may manifest in various ways, including wishing to dress and present themselves as the desired gender.
Significant incongruence should exist between the individual’s experienced or expressed gender and their assigned gender. This gender incongruence must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The diagnostic criteria require that these feelings of incongruence and distress be present for a significant duration, typically at least six months. This criterion helps distinguish between transient gender exploration and more persistent experiences of gender dysphoria.
Mental health professionals must rule out the possibility that the distress is due to another mental health or medical condition. Conditions like schizophrenia, where delusions of gender identity may occur, must be considered.
Diagnosing gender dysphoria is a multidisciplinary process that involves several mental health professionals working together to provide comprehensive care. Here are the key professionals involved:
Psychologists and psychiatrists play a central role in assessing and diagnosing gender dysphoria. They conduct clinical interviews and assessments to understand the individual’s gender identity, explore co-occurring mental health conditions, and evaluate the persistence and severity of dysphoric feelings.
Licensed therapists and counselors provide ongoing support and therapy to individuals with gender dysphoria. They help clients cope with distress, navigate the challenges of gender transition, and address any mental health concerns that may arise during the diagnostic process.
In cases where individuals pursue medical interventions like hormone replacement therapy (HRT) or gender-affirming surgeries, endocrinologists play a vital role. They assess the physical and hormonal aspects of gender transition, monitor hormone levels, and manage associated medical concerns.
Pediatricians and adolescent medicine specialists can contribute to the diagnostic process for children and adolescents with gender dysphoria. They assess physical development, guide families, and collaborate with mental health professionals to ensure appropriate care.
The diagnostic process for gender dysphoria is comprehensive and patient-centered. It involves several steps to ensure an accurate diagnosis and to provide individuals with the necessary support and care:
The process begins with an initial assessment and clinical interview conducted by a mental health professional, typically a psychologist or psychiatrist. During this interview, the individual discusses their feelings, experiences, and history related to gender identity.
A psychological evaluation may include standardized assessments and questionnaires that help quantify the individual’s distress and the extent of gender dysphoria. This evaluation aims to measure the individual’s psychological well-being objectively.
The mental health professional explores the individual’s gender identity, including their preferred name, pronouns, and the extent of their desired gender expression. This exploration is conducted in a supportive and non-judgmental manner, respecting the individual’s autonomy and self-identification.
Assessing co-occurring mental health conditions is crucial as they can impact the diagnostic process and treatment planning. Mental health professionals must address depression, anxiety, or substance abuse.
Once a diagnosis of gender dysphoria is confirmed, mental health professionals collaborate with the individual to create a personalized care plan. This plan may include psychotherapy, hormone therapy, and, in some cases, gender-affirming surgeries. It ultimately depends on the individual’s preferences and medical suitability.
Cultural competence and sensitivity are integral to the diagnostic process for gender dysphoria. Mental health professionals must be attuned to the unique experiences and challenges faced by transgender and gender-diverse individuals. This includes respecting the individual’s chosen name and pronouns, understanding cultural factors that may influence their identity, and providing a safe and affirming environment for disclosure.
Diagnosing gender dysphoria is a complex but essential process that involves a careful assessment by mental health professionals. The diagnostic criteria outlined in diagnostic manuals help ensure a standardized approach to diagnosis. At the same time, a multidisciplinary team of professionals collaborates to provide comprehensive care.
Through culturally competent and patient-centered evaluation, individuals with gender dysphoria can receive the support and treatment they need to navigate their gender journey and achieve better mental health and well-being. As our understanding of gender diversity evolves, mental health professionals must continue to adapt their diagnostic and treatment approaches to meet the diverse needs of this population.

Discover the Best Age to Start Gender Reaffirmation With HRT and take a step closer to your authentic self. Hormones are essential for both developing and maintaining characteristics related to gender. At HEALOR ™ transgender care clinic in Las Vegas, our compassionate team is pleased to offer hormone replacement therapy (HRT) to help patients of all needs and backgrounds begin their gender reaffirmation journey. During this time, board-certified physician Dr. Raj Singh believes it's important that you feel fully informed and prepared.
One common question people have about gender reassignment is when to start HRT. Some people say the best age to start is as early as 16, while others make the decision later in life. Because there are no set guidelines, the decision should be made with careful consideration of what would work best for you. If you want to know the pros and cons of HRT, call our Las Vegas, NV clinic for a discussion.
Hormone replacement therapy is the process of changing the hormone levels in your body. During treatment, estrogen or testosterone can be administered through injections, pills, or topically. This is performed for transgender individuals who would like to transition their physical appearance, so it better aligns with their gender identity.
For example, estrogen can be used for more feminine characteristics, like breast development, while testosterone is for more masculine traits like facial hair. In a gender reaffirmation consultation with the providers at HEALOR ™ transgender care clinic in Las Vegas, we can learn about your goals and create a personal treatment plan for hormone replacement. We're here to make your journey as smooth as possible.
Many of our patients want to learn the pros and cons of HRT at an early age. Here are some well-known benefits of hormone replacement in Las Vegas, NV:
There is some debate about what age to start hormone replacement therapy. Some people start at 16 because many medical professionals agree that the teenage years may be easier to transition through. By starting hormones during adolescence, transgender people can begin making immediate changes.
However, it's also normal for people to wait until later in life to begin their transition. If you aren't having difficulties with your assigned gender, then there's no need to rush into something that may be challenging or painful for you. At our clinic, we believe the best age is based on an individual's maturity and understanding of the process.
If you're still uncertain or hesitant about what age to start hormone replacement therapy, Dr. Singh and the trusted team at HEALOR ™ transgender care clinic in Las Vegas can answer your questions and guide you on the path to treatment. Whether we see you for an initial gender reaffirmation consultation or as a returning patient, our providers are here to support you. We're proud to have worked with many transgender people in their personal journeys.
You may wonder if there's a "best age" to start hormone replacement therapy. If you're considering transitioning, the best time to start hormones is on your timeline. If you want more information about the pros and cons of HRT from a board-certified physician, call Dr. Raj Singh for a hormone assessment in Las Vegas, NV. The compassionate staff at HEALOR™ transgender care clinic is ready to get started with you.
Questions about the best form of estradiol therapy for Feminizing hormone therapy?
Feminizing hormone therapy with Estrogen is a treatment that can be utilized to help alleviate the symptoms of gender dysphoria. Often it's combined with progesterone and testosterone blockers, which can help transition more smoothly
For some people, feminizing hormone therapy is an important part of their journey to authenticity. The goal for this type of treatment would typically be inducing physical changes that match gender identity and expression- like developing breasts or less facial hair.
For example:
Reduction in facial hair, most individuals will notice a decreased need to shave. For best results, we recommend laser hair removal or electrolysis. Laser hair removal may be the perfect solution for some individuals to reduce their need or desire in shaving. Laser treatments work by targeting and destroying hairs with high-energy light, while electrolysis uses an electric current that causes pores on your skin to strip away cells creating space between follicles causing them to die off over time.
The process of redistribution, or storing fat into different areas can cause a woman's figure to develop. Estrogen is what causes this change in shape because it increases the storage and development of body fats throughout your entire system - including breasts as well as hips. Here is a detailed article to address the development of breasts with hormone therapy
Before treatment can be started we require:
Some providers are using much higher doses of estradiol therapy in an attempt to accelerate feminization. There is no data supporting this practice, however. The duration of hormones is an important factor to consider when it comes to physical changes. Hormone therapy can take up to 2 years before you start seeing maximal results, and those who use them for a long enough period will notice that their voice may change over time. We discourage the use of high doses and supraphysiological levels of estrogen as this can lead to significant side effects such as a risk increase in blood clots, cancers, anxiety/depression, and heart disease.
This is the mainstay of Feminizing hormone therapy. Estradiol is a steroid sex hormone that is produced by the ovaries and adrenal glands in biological females. Individuals who are overweight also tend to have a conversion of testosterone to estrogen in body fat by an enzyme called aromatase. Estrogen therapy also helps suppress the production of androgen such as testosterone.
Have more questions? Schedule a consultation with one of our licensed providers to get started.

Eating disorders are difficult for anyone, but they affect transgender people differently and harshly. Trans people have a very high prevalence of eating disorders due to our intersecting mental health difficulties, and we deserve treatment all the same. Stick with me for a discussion about this important topic, and learn some ways to care for nutrition during transition.
A quick intro: Hi, I’m Summer and I’m HEALOR™ new blog writer. I hold a Master’s in Psychology, and I’m keenly interested in wellness, mental and physical. For my first piece, I’d like to explore an under-discussed topic that’s pretty close to my heart.
Eating disorders are an umbrella of experiences and diagnoses involving eating habits that are damaging to well-being. They appear in many thought patterns and behaviors and do not always correspond to high or low body weight. Many people who have eating disorders appear ‘healthy’ but experience serious emotional distress. Once the disorder progresses, it can weaken the immune system, worsen mental health, and permanently damage the vital organs.
Eating disorders are strongly related to self-esteem, social settings, and feelings of control. Many disordered behaviors involving food can be traced to a loss of control or an intense desire for control. These are often tied to cultural expectations of how a person ‘should’ look in their family or society.
While not all transgender people experience gender dysphoria, most of us do. Gender dysphoria often manifests as a negative feeling about our appearance. Gender dysphoria is also a massive contributor to depression and anxiety, which can disrupt our self-image and eating patterns. There are also emotional consequences to being transgender in the face of discrimination: we often have a punishing desire to be read as our gender (or ‘pass’) so that we can live peacefully. We’re also influenced by expectations of how cis and trans people ‘should’ look in media and society.
To recap: our self-esteem is often shaken and tied to a desire to change our bodies. We are at enormous risk of depression and anxiety. We live with high social pressure to change ourselves for the benefit of others. For these reasons, being transgender places us in a perfect storm of risk for eating disorders.
Short answer: yes!
Most research into eating disorders is done on cisgender people. It also prioritizes the young, cis women who make up the majority of diagnoses. This isn’t unreasonable, but the data has left trans people behind.
Eating disorders are very gendered, and trans people experience gendered expectations and roles differently to cis people. Cisgender American women are diagnosed more than twice as often as men for anorexia and bulimia nervosa but are by no means the only people affected.
Where trans people differ is that we experience eating disorders alongside the bodily dissatisfaction of gender dysphoria and other mental health challenges. This leads to higher rates of eating disorders among adolescent and young adult trans people. Our situation is made worse by the fact that treatment can be very trans-exclusionary.
Some of the ways these disorders can manifest in trans people are:
It’s important, to be honest, and willing to ask for help. Eating disorders thrive on dishonesty: they fill our minds with falsehoods about how we look, and how we ‘should’ look to be more valid human beings. They prey on our anxieties and trauma to warp our self-esteem. Mental distress like anxiety, depression, and eating disorders are insidious because they damage the ability to self-assess our well-being or make recovery decisions. Mental distress is punishing because it damages our agency.
If you see warning signs like a strong interest in modifying body weight or starting heavy, unsupervised exercise, it’s good to seek other opinions. Healthy weight loss is possible, but it is best done with medical supervision. If you're interested, read resources from advocacy groups to see if your feelings align with eating disorders. If you have a GP or therapist, consult them for an expert opinion.
Remember that eating disorders aren’t just about weight. They’re about emotional distress and control (or loss of control). Distressed thoughts and behaviors merely become a vehicle for the bodily changes. Managing weight without addressing the underlying thought patterns is often unsustainable. Recovering from harmful mental patterns can bring wholesome well-being, even if bodily health takes time to follow.
Reflect on your eating as part of your collective well-being. Disruptions in eating or sleep are one of the first signs that something is amiss and there’s a reason that doctors ask about them. Reflection is really important for dysphoric trans people impacted by dysphoria and other mental stressors. Ask yourself if you’ve been eating as much as you’d like to. Ask yourself if you’re comfortable with how much you eat. Ask yourself if other stressors in your life are challenging your self-esteem.
And lastly, remember the difference between healthy and unhealthy desires. Most trans people are familiar with the dreadful assertion that being transgender is something that needs to be 'treated'. Having gender dysphoria and an eating disorder can entrench this because the dysphoria and eating disorders often stem cast similar shadows. Both stem from profound disruptions in self-esteem and bodily satisfaction, and both come with a strong desire for changing oneself.
The reason that eating disorders should be countered and transition should be supported is a fundamental difference in outcomes. The natural outcome of letting a well-supported gender transition is a happier, more vibrant person. The natural outcome of an unmanaged eating disorder is physical and mental deterioration, with a high risk of death. The harms of transition are often attached to discrimination and healthcare denial. The harms of eating disorders are societal and psychological. Always remember that your gendered self is valid, with or without the challenges that accompany it.
Seek help when the time is right. Once you feel ready to talk to a clinician about your eating habits, don’t hesitate to make the call. Like any form of mental distress, earlier is better for long-term care. Mental distress isn’t always treatable through medicine alone, and disordered eating is a star example of this. The best cases of recovery come from dedicated clinicians, social support (family and friends), and personal effort. Recovery isn't a slope of continuous progress, either. It's full if missteps, relapses and learning.
But from someone in recovery – it’s never too late to try.
Note: This article was reviewed by Dr. Raj Singh prior to publication.

Hormone Disorders and Their Impact on Transgender Hormone Therapy
Hormone disorders can impact transgender hormone therapy by affecting the body's ability to absorb, metabolize, and utilize the hormones administered. Hormone disorders can occur when the body produces too much or too little of certain hormones or when there is an imbalance in the levels of hormones in the body. This informative article will discuss thyroid disorders, polycystic ovary syndrome (PCOS), adrenal disorders and hypogonadism and their effect on transgender hormone therapy.
Polycystic ovary syndrome is associated with increased ovarian production of androgens such as testosterone, typically between ages 15-45. There is also an increased rate of anxiety and depression with PCOS.
Masculinizing hormone therapy is a medical treatment used to induce masculinization in transgender men or gender non-conforming individuals who wish to achieve a more masculine appearance or gender identity. This typically involves testosterone therapy, which can help promote the development of male characteristics such as cessation of the menstrual cycle, facial and body hair growth, a deeper voice, and increased muscle mass.
Masculinizing hormone therapy typically will begin producing changes in your body within weeks to months. In individuals with PCOS, the timeline of these changes may differ from those without PCOS.
Although this is an area of limited research, recent data has shown that starting testosterone therapy does not exacerbate PCOS symptoms and may help improve some of the metabolic problems associated with PCOS.
Thyroid disorders are conditions that affect the function of the thyroid gland, a butterfly-shaped gland located in the neck that produces hormones that regulate metabolism and other bodily functions. The two most common thyroid disorders are hypothyroidism and hyperthyroidism.
Hypothyroidism occurs when the thyroid gland does not produce enough thyroid hormone, slowing the body's metabolic processes. This can cause fatigue, weight gain, constipation, dry skin, and cold intolerance.
Hyperthyroidism, on the other hand, occurs when the thyroid gland produces too much thyroid hormone, accelerating the body's metabolic processes. This can cause symptoms such as weight loss, rapid heartbeat, anxiety, sweating, and tremors.
Transgender HRT with estrogen can have a higher incidence of hypothyroidism than the general population. Estrogen therapy is associated with increased production of thyroid-binding globulins (TBG), which bind to thyroxine or T4 and prevent conversion to the active or free form of thyroid hormones called Tri-Iodothyronine or T3 hormone. The net result is the thyroid produces more T4 to compensate for this effect. This can overstress a weak thyroid gland and cause long-term hypothyroidism issues.
Individuals on estrogen-feminizing therapy can have typical symptoms of hypothyroidism. However, thyroid-binding globulin levels are not routinely checked, and thyroid hormones can remain normal. This often results in an undiagnosed or undertreated thyroid problem and may exacerbate underlying depression and chronic fatigue in transgender patients. Transgender individuals on estrogen therapy with symptoms of hypothyroidism should request their doctor to order thyroid-binding globulin (TBG) and free thyroid hormone (FT4, FT3) levels to diagnose this condition.
Hypothyroidism is also associated with high total testosterone and low free Testosterone levels, possibly due to increased production of sex hormone binding globulin ( SHBG ) by the liver. This results in too much bound or inactive form of testosterone. Transgender men with untreated hypothyroidism can require higher doses of testosterone to achieve the desired results, which may result in accelerated aromatization to estrogen and a higher percentage conversion to dihydrotestosterone (DHT) which can lead to adverse effects.
Just like hypothyroidism, individuals with hyperthyroidism can have high total testosterone and low free Testosterone levels, (area of debate) associated with significant elevations of the mean total testosterone and sex hormone-binding globulin (SHBG) levels and significant reduction of free Testosterone.
In addition, elevated estradiol levels and enlarged breasts (gynecomastia) are common in hyperthyroidism, which can negatively impact a transgender person's masculinization journey.
The adrenal glands are two small, triangular-shaped glands located on top of the kidneys. They play an important role in regulating various bodily functions, including metabolism, blood pressure, immune system function, and the body's response to stress.
Disorders of the adrenal glands can occur when these glands produce too much or too little of certain hormones, leading to a wide range of symptoms and health problems. Some common adrenal disorders include:
A condition in which the adrenal glands do not produce enough cortisol and aldosterone, leading to symptoms such as fatigue, weight loss, low blood pressure, and electrolyte imbalances.
Antiphospholipid antibody syndrome (APL) is a potential cause of Addison's disease. APL is a condition where individuals have a higher risk of developing blood clots. This can be particularly concerning for transgender women who are undergoing estrogen therapy, as they may be at an increased risk for blood clots and other complications.
Adrenal glands, also produce prohormones like dehydroepiandrosterone (DHEA) and DHEA sulfate. People with Addison's disease may experience low libido and chronic fatigue due to the lack of these hormones. While DHEA supplementation can help alleviate these symptoms and improve overall well-being, it can also complicate hormone therapy for transgender patients with Addison's disease. This is because DHEA can be converted into testosterone and estrogen, which can interfere with hormone therapy management.
is a genetic disorder that affects the production of adrenal hormones, leading to symptoms such as abnormal genitalia, infertility, and electrolyte imbalances. In some cases, CAH can also affect the production of sex hormones, leading to variations in gender identity and sexual development. Individuals with CAH may experience differences in gender identity and sexual orientation, as well as physical changes such as ambiguous genitalia or early onset of puberty.
Some individuals with CAH may identify as transgender or may seek gender-affirming treatments such as hormone therapy or surgery. For transgender individuals with CAH, hormone therapy can be complicated due to the underlying hormone imbalances associated with the condition. Testosterone therapy for transgender men with CAH may increase the production of androgens, which can exacerbate symptoms of CAH such as acne and excessive hair growth. Similarly, estrogen therapy for transgender women with CAH may exacerbate symptoms of CAH such as menstrual irregularities and electrolyte imbalances.
Hypogonadism is a condition in which the body does not produce enough of the sex hormones testosterone and/or estrogen. For transgender individuals undergoing hormone replacement therapy (HRT) as part of their gender transition, hypogonadism may be a concern. This condition requires lifelong treatment with either testosterone or estrogen, depending on the individual's gender identity. Due to the lack of hormone production by their native glands, higher doses of hormones may be necessary to achieve the desired physical changes. Pellets are a form of hormone therapy that offers a unique advantage over other methods such as injections, gels, or oral medication. They provide long-term hormone therapy, making them an attractive option for those with hypogonadism.
The relationship between PCOS and gender euphoria is complex and multifaceted, and the experience of gender identity and euphoria is unique to each individual. It is important to understand that not all individuals with PCOS identify as transgender or experience gender euphoria. However, for some transgender men with PCOS, the physical changes that come with the condition may align with their gender identity and be affirming.
As this is a relatively unexplored topic, I have made every effort to ensure the accuracy of the information presented. However, I welcome any feedback or differing opinions you may have. Please feel free to share your own experiences and thoughts by leaving a comment below.
Thanks for Reading!
Raj Singh MD, FACP, FASN

I am often asked what we can expect in terms of breast development after starting estrogen therapy by a many of of my transgender patients. This is an area of very limited research and I will do our best to shed some light on this topic
Normal breast development: breast development is a complicated process that starts at birth in biological females and then accelerates during puberty.
There are 5 stages of breast development in biological females and transgender women. The timeline of breast development in transgender woman can vary significantly depending upon the age, dose and duration of feminizing hormone therapy with estrogen. There can also be variation depending upon the type of estrogen modality used such as oral estradiol versus topical, estradiol injection or estradiol pellets.
| Stages | Timeline | Changes |
| Stage I | 3-6 months | Tip of the nipple is raised |
| Stage II | 6-12 months | Breast buds appear, both the breast and the nipple gets enlarged. A dark circle develops around the nipple which is called areola. |
| Stage III | 12-16 months | Further enlargement of the breast tissue |
| Stage IV | 2-3 years | Elevation of the nipple and the breast and increase in size of areola |
| Stage V | Transgender women are unlikely to achieve this stage. Surgical breast implants are required if a larger breast size is desired. |
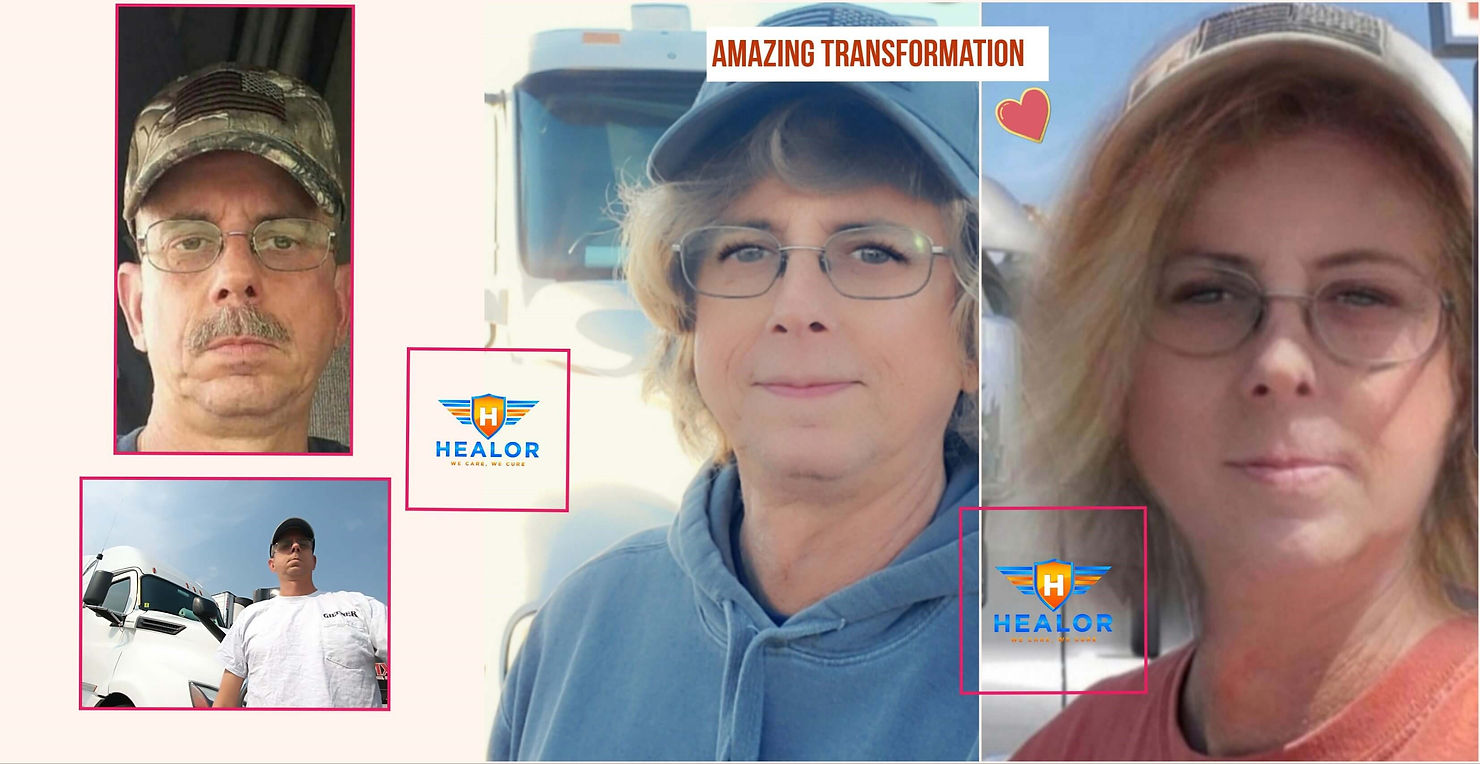
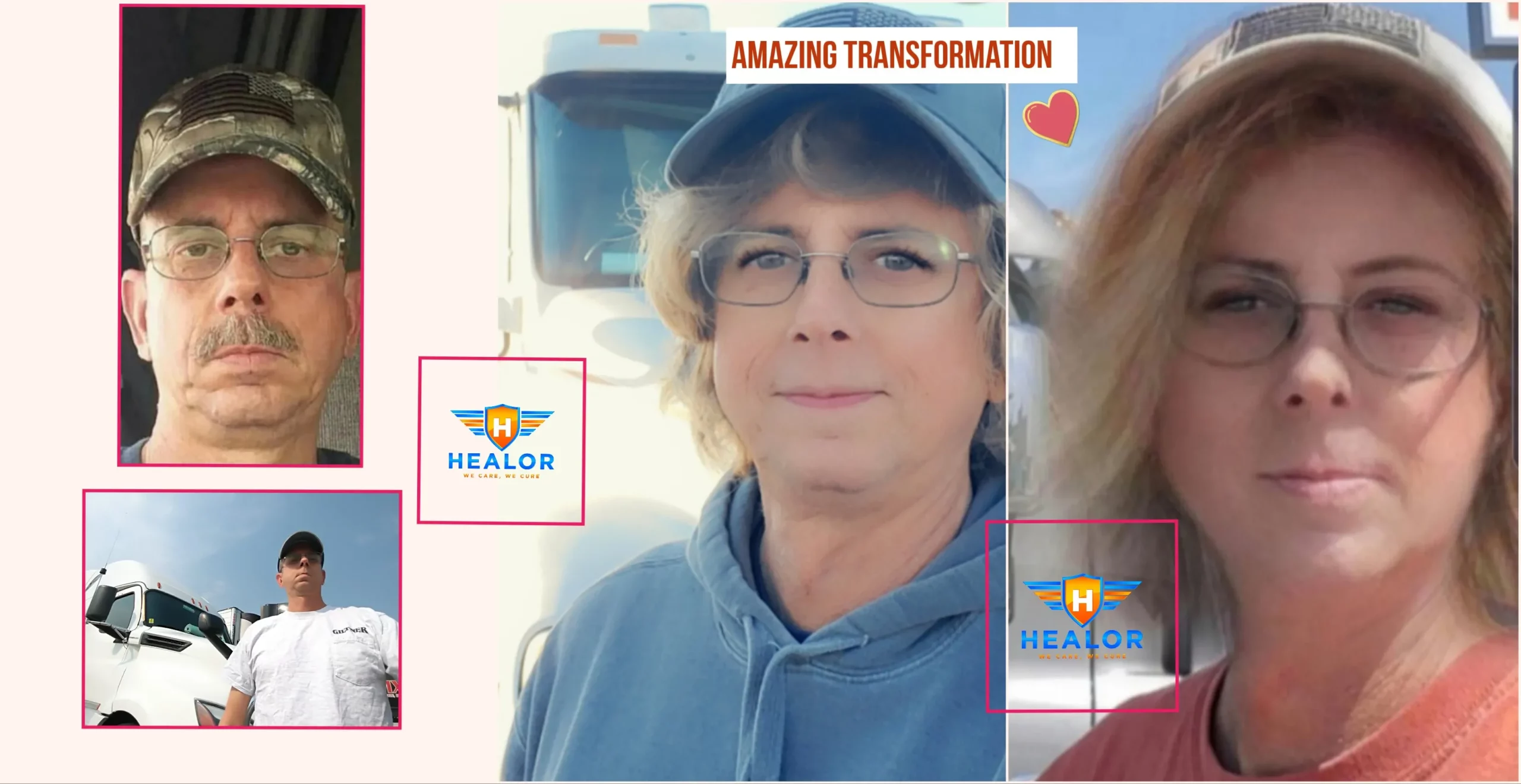
Transgender women MTF Transition Pictures
We are sincerely thankful to our patients for allowing us to use their transition pictures to help guide others in their journey.
Progesterone therapy is recommended for transgender patients to decrease the negative side effects of estrogen. In my personal opinion, Progesterone supplementation does not significantly change the development of breast tissue.
Testosterone suppression with anti androgen such as spironolactone, bicalutamide, finasteride or additional medications are required to augment breast development. Elevated testosterone levels have a negative effect on breast tissue development and ideally should be maintained below 100 ng per dL.
Dr. Raj Singh MD, FACP, FASN
Starting transgender hormone therapy can be overwhelming, but it doesn't have to be. Get your questions answered with this list of the top 9 transgender hormone therapy FAQ.

At HEALOR™, we have treated hundreds of patients with gender dysphoria and based on our experience we have compiled a list of the most commonly asked questions when it comes to Feminizing or masculinizing hormone therapy.
As most hormone therapies can have irreversible effects both physically and mentally, we at healor, require a letter or statement from the patient's psychiatrist or counselor before Feminizing or masculinizing hormone therapy can begin. This is in compliance with Nevada state law. Regulations and laws vary across different states and we encourage you to discuss this with your medical provider.
In female to male transition, you can expect enlargement of the clitoris, deepening of the voice, increase in facial and body hair, irregular menstrual cycles followed by complete cessation of the menstrual period, and a decrease in the percentage of body fat. In male to female transition, you can expect a decrease in testicular size, decreased erections, an increase in percentage body fat, and some growth of breast tissue.
Testosterone therapy can increase the production of sebum which makes the skin to be more oily which can result in the development of acne and flare-up of acne.
Scalp Hair loss is very variable, as the sensitivity of hair follicles to dihydrotestosterone or DHT may vary. Patients who are on higher doses of testosterone will experience male pattern baldness. We at healor, will prescribe customized formulations containing finasteride to block DHT conversion, which protects scalp hair from damage. we do not recommend oral finasteride due to the risk of irreversible sexual dysfunction.
Patient’s on masculinizing hormone therapy can expect complete cessation of the menstrual cycle in 6 months.
Deepening of voice on masculinizing hormone therapy generally takes about 6-12 months and is irreversible.
Growth of Breasts varies on the age of the client, estrogen levels, and appropriate use of androgen blockers for best results. Among Anti Androgen drugs, Bicalutamide tends to have the most effect on breast growth, however, this medication can cause liver enzyme elevation and must not be used in individuals with liver problems The development of breast tissue is variable, typically results are seen in about 3 months and breast tissue growth may continue for up to 2 years. Many patients are happy with the results, however, some may require surgical breast augmentation. Read this blog titled " Breast growth with Estrogen Therapy in transgender patients" for more details on this topic.
Patients can experience male pattern baldness, the development of acne, increase in red blood cell production which can raise hemoglobin levels and cause secondary polycythemia. Secondary polycythemia can increase the risk of heart disease and stroke. Some other risks include the development of osteopenia and osteoporosis, the elevation of cholesterol and liver enzymes.
Patients can experience More blood clots, the elevation of liver enzymes, elevation of lipids especially triglycerides and breast cancer.
I hope this was helpful in improving your understanding of hormone therapy.

Curious Will Testosterone Make Trans Men More Masculine?
Transitioning is an important decision for many of our patients at HEALOR™ in Las Vegas, NV. Whether you’re deciding to do a female to male transition or a male to female transition, it’s important to work with an experienced doctor, like double board-certified physician Dr. Raj Singh. He has worked with the LGBTQ community for years and has helped them start their gender affirmation journey, and provided other LGBTQ health services.
Gender dysphoria is the belief that someone’s identity doesn’t match their biological sex. This can lead to anxiety and depression over time. Those with gender dysphoria often choose to transition to their preferred gender. We provide consultations to help patients learn if they’re a candidate for transgender hormone therapy. For patients wanting a female to male transition, we will use testosterone treatment. During this visit, we will learn if you’re healthy enough for this hormone replacement treatment.
Transgender hormone replacement therapy involves administering different hormones to help patients acquire the look of their preferred gender. For patients wanting a female to male transition, this involves testosterone. At HEALOR™, Dr. Singh offers a safe space for patients receiving hormone replacement therapy. We administer hormones through pills, topical creams, or even by injection.
Dr. Singh is highly-trained and experienced with hormone therapy and can determine the proper method and dosage for each patient at his Las Vegas, NV office. Your results occur over time. We like to start with low dosages to make sure your treatment is as safe as possible. Many of our patients experience changes in their appearance in six months to a year after starting transgender hormone therapy.
Ultimately, each patient can experience different ftm testosterone effects from hormone replacement therapy. Some common physical effects of this therapy include:
During your visit, Dr. Singh can discuss these physical changes, so you will be aware of them before they occur.
When you’re considering testosterone therapy in Las Vegas, NV, you may have questions about the process. Here, we address some of the most commonly asked questions received at HEALOR Primary Care about hormone replacement therapy.
Yes, at HEALOR Primary Care, we do require a letter of statement from a psychiatrist or counselor before you can begin this hormone replacement therapy.
2. When will I stop having my period?
Patients going through ftm testosterone therapy can expect cessation of their period in about six months.
3. What are some risks for a female to male transition?
Some patients may experience male pattern baldness, elevated cholesterol or liver enzymes, and an increased red blood cell production or secondary polycythemia, which increases their risk of stroke or heart disease.
At HEALOR™, we offer compassionate and confidential care for the LGBTQ community looking to transition safely. Dr. Raj Singh is well-versed in hormone replacement therapy, including testosterone therapy, and can help his patients transition from female to male or from male to female. If you want to learn more about transgender hormone therapy, call our Las Vegas, NV office to schedule an important consultation.

Bicalutamide is an anti-androgen drug which means that it blocks the effect of androgenic hormones such as testosterone and DHT. The important thing to understand is that bicalutamide does not lower testosterone levels, it simply blocks the effect of testosterone on tissues. In many cases, Testosterone levels initially increase after starting this medication however, that is nothing to be concerned about. Testosterone levels start declining over time, this change happens much more rapidly if you're also taking estrogen and progesterone in addition to bicalutamide
Bicalutamide is most commonly used for treating men with prostate cancer
Off-label uses:
Today primarily will be focusing on bicalutamide use in transgender females
Other anti-androgen medications often prescribed are spironolactone and cyproterone acetate. However, these drugs are much weaker than bicalutamide. Cyproterone is also not available in the US.
Bicalutamide also helps the aromatization of testosterone to estrogen which is why it is especially helpful for breast development when compared to other anti-androgen medications. Some small studies have shown better breast growth when compared to Aldactone and cyproterone. A possible mechanism is that Aldactone causes early maturation of the breast bud when compared with bicalutamide.
Comparison of anti-androgen effect of bicalutamide, Aldactone, and Cyproterone in transgender females.
Bicalutamide is known to cause a reduction in vitamin C levels and glutathione levels in animal studies. Taking glutathione and vitamin C may reduce the risk of liver toxicity however I have no data to support this strategy.
Half-life is 6 days so the drug stays in the body for several days so only twice a weekly dose is adequate. Compare that to spironolactone which has a half-life of only 2 hours
Do not use or use caution if you
Get a liver panel done 2-4 weeks after starting the medication. For any sign of liver failure such as jaundice, the medication must be immediately stopped.
Bicalutamide stays in the body for several days and has a half-life of 6 days which means half of the drug is broken down and removed by the body in 6 days. Twice a weekly dose of 50 mg is adequate. Higher doses increase the risk of liver toxicity and should be avoided
In summary, this is a very good medication for feminization therapy especially if high breast growth is strongly desired. Liver toxicity is a major concern and can be life-threatening so do not consume alcohol, and avoid hepatotoxic medications such as Tylenol.
Gender identity is an innate sense of feeling different than one’s anatomy. Estrogen Hormone Therapy is a possible way to transition from a male to a female. People want the changes from hormone therapy to happen rapidly, but there are some expectations, long-term considerations, medications, and other factors that need to be understood. These factors can include genetics, a person’s age when taking the hormone therapy, and the overall state of health of a patient.
There are four main stages that the changes happen in as the Estrogen Hormone Therapy continues.
As Estrogen Hormone Therapy progresses, the skin can become thinner and drier. Pores produce less oil and become smaller. You may notice that you develop cuts or bruises more often and the odor from your urine and sweat change. You may sweat less as well.
You may experience temperature and pain differently due to a difference in touch. Small ‘buds’ can develop under the nipples within a few weeks. Touching them may result in slight pain, and they can also look uneven. This is a normal process for breast development, and the pain will diminish over the next few months. The size and shape of the breasts can vary from person to person.
The body also begins to redistribute fat to different parts of the body. Fat will collect around the thighs and hips while the muscles on the legs and arms will look less defined. Strength and muscle mass will also decrease, which is why at HEALOR ™ we recommend exercising to maintain general health and muscle tone.
The face and eyes also look more feminine as the fat shifts or increases. It may take a few years to develop, which is why it is better to wait at least two years before you take any drastic feminization steps via procedures.
The hair on the body, including arms, back, and chest will grow less thick. Their growth will also slow down with time. Facial hair will also grow slower and thin out. However, it will not go away completely without laser treatments and electrolysis.
Some people also notice changes in height or shoe size, but this is very minor.
Changes in the emotional state vary according to the person. The transition is often similar to puberty and feels like a roller coaster. You may feel like you are experiencing more feelings or emotions and even developing different pastimes, tastes, interests, and behavior in relationships. If these changes are affecting the quality of life then we generally will discuss reducing dose of Estrogen. Some people may need supportive psychotherapy during these changes.
After beginning Estrogen Hormone Therapy, you will notice that the number of erections you experience has lessened. It may also not be firm enough or last long enough to penetrate. However, you will be able to experience orgasms and even have erotic sensations.
Some people also find that different parts of the body and sex acts are pleasurable now. Orgasms can have less peak intensity and begin to feel as though they impact the whole body rather than just the genitals. People may have ejaculations with white or clear fluid or even none at all. Exploring and experimenting with this newfound sexuality and body through sex toys and vibrators can be great, as well as involving a significant other.
The testicles can also shrink to half their original size.
Within a few months of Estrogen Hormone Therapy, you should assume that you are irreversibly and permanently sterile. Some may maintain a sperm count or have their sperm count return to normal after stopping Estrogen Hormone Therapy, but that is a very rare occurrence.
If you want to have children through your own sperm, you can speak to us at HEALOR about preserving your sperm before starting this therapy. While you are on the hormone treatment and have sex with a woman who can become pregnant, it is a good idea to use birth control.
The hormone estrogen influences most feminine characteristics. It can be given by pill, injection, or skin preparations like patches, sprays, gels, and creams. Pills are effective, cheap, and convenient, but if you’re older than 35 or smoke, their safety can be compromised. Patches are also safe and effective, but you will need to wear them all the time. They can also irritate the skin. We generally start Estrogen at a dose of 2 mg/day and titrate the dose to achieve the desired results while limiting adverse side effects.
Most transwomen take in estrogen via injection. Injections can cause fluctuating or high estrogen levels, resulting in weight gain, mood swings, anxiety, migraines, or hot flashes. There isn’t much information with regard to taking high levels of estrogen over a long time.
Contrary to popular belief, relatively small doses of estrogen can actually have the most effect on the transition. Higher doses don’t necessarily make the changes happen quickly and may even harm your health. After going through orchiectomy (the removal of testicles) or genital surgery, the estrogen dosage should be lowered by the doctor. Without testicles, you will need less estrogen for good health and feminine characteristics.
You will periodically need to get liver function, cholesterol, and diabetes screenings to check on your health while on estrogen.
The risks of strokes, cancer, and blood clots are small but do increase. Doctors do believe that the risk of prostate cancer may go down, but there isn’t enough scientific evidence for this. It is better to follow standard testing guidelines according to your age. The risk of breast cancer can slightly increase but still remains lower than that of a non-transgender female. After 2-3 years of Estrogen Hormone Therapy, it is a good idea to get breast cancer screenings, depending on your age and risk factors.
There hasn’t been a lot of research on the use of estrogen by transwomen. This is why there may be other risks that may exist that doctors aren’t aware of. This is especially true for transwomen who have been using estrogen for many years.
At the end of the day, it is important to consider all the different changes you will go through with a clear mindset. Transitioning is an important step for anyone, and proper care should be taken with your health as you go through it.
Transgender health and Transgender hormone therapy is a highly specialized field and it is important to find a transgender clinic that has experience in managing hormone therapy for transgender patients.

Transitioning is one of the most significant life decisions you can make. Whether you decide to transition from male to female or female to male, meeting with a supportive and knowledgeable doctor you can trust is crucial. Double board-certified physician Dr. Raj Singh frequently works with the LGBTQ community so patients can begin their gender affirmation journey as soon as possible.
So what is transgender hormone therapy? By administering certain hormones in individuals, they acquire the characteristics of their preferred gender. If you are interested in this therapy, you are in good hands. HEALOR™ is committed to providing a safe space for patients to receive the care they need. Learn about transgender hormone therapy in Las Vegas, NV, by calling our clinic for a consultation.
Gender dysphoria involves a strong sense that a person's gender identity does not match their biological sex. This may lead to feelings of depression, anxiety, or discontentment that interfere with your daily life. Individuals with gender dysphoria often decide to transition to their preferred gender. If so, you may be a candidate for transgender hormone therapy. This is also called hormone replacement therapy (HRT).
You should attend a consultation with Dr. Singh to determine if HRT is the right way to move forward. We can determine if you are healthy enough for treatment by asking about your medical history and family background. We may also run a few tests to understand which treatment path and hormones work best for your needs. HEALOR understands this is a significant decision and hopes to make your appointment as comfortable as possible.
So what is transgender hormone therapy? Treatment may look different based on your needs and personal goals. For example, transgender men may receive testosterone, while transgender women may receive estrogen. Hormones are generally administered through injections, pills, or a topical cream. With our deep understanding of hormone therapy, the professionals at HEALOR™ can determine the appropriate method and dosage.
Patients should know that the results from HRT occur gradually over time. Dr. Singh usually suggests low dosages to guarantee the safest treatment possible. The great news is that many people report seeing the desired changes in their appearance six months to one year after beginning transgender hormone therapy in Las Vegas, NV. You may also notice changes to your reproductive system or sex drive. If you have concerns, feel free to contact a member of our caring team. We can review all of your questions together.
At HEALOR™ , we are committed to providing compassionate, state-of-the-art care for the LGBTQ community. Double board-certified physician Dr. Raj Singh promotes an environment of trust to address the needs of every individual. Our entire staff is dedicated to providing comprehensive treatment options for various needs. If you have gender dysphoria or want to learn more about hormone replacement therapy, we encourage you to contact our facility in Las Vegas, NV. We can help you take the next big step.

Can Transgender Hormone Transition Therapy Be Reversed?
At HEALOR™, we know how meaningful and exciting it is to move forward with gender transitioning and become the person you were always meant to be. Transgender hormone therapy is an integral part of gender dysphoria treatment, whether it takes place in the pre-surgical phase of the process or as a standalone approach. Double board-certified physician Dr. Raj Singh MD has advanced expertise in hormone replacement therapy (HRT) and has guided numerous patients in the Las Vegas, NV LGBTQ community throughout their gender reaffirmation journeys.
Before moving forward with this treatment, it is important to understand whether or not transgender hormone transition therapy can be reversed. Taking feminizing or masculinizing hormones will have a physiological and emotional impact, and we want to ensure you are fully aware of how this process will affect your body, health, and quality of life. Dr. Singh and our caring team are here to provide the information you need and will be with you every step of the way.
Transgender hormone replacement therapy is the administration of hormones to help patients acquire the physical characteristics of their true gender. Feminizing hormone therapy is administered to individuals who wish to transition from male to female (MTF) and involves taking estrogen, progesterone, and testosterone blockers such as Aldactone, bicalutamide, and cyproterone acetate.
Female-to-male (FTM) transition patients receive testosterone throughout the course of their hormone replacement therapy. Hormones may be taken via oral pills, injections, or absorbed through the skin via a transdermal patch or topical cream. Another novel approach we utilize is insertion of hormone pellets under the skin. Hormone pellets provide several months of treatment without the inconvenience of pills, or pain associated with injection therapy.
The effects of transgender HRT take place over time. While some are irreversible, many components of transgender hormone therapy for Las Vegas, NV patients can be reversed when the hormones are no longer administered. However, the extent to which a person might experience such effects is largely dependent upon the length of time the hormones have been taken, genetics, and other factors. During your consultation at HEALOR™ , Dr. Singh can talk with you about these effects and answer any questions you have.
Many of the physical characteristics that result from transgender HRT taken to block testosterone production in the body (in trans women) may diminish or be reversed when the hormones are no longer taken. Some of these include:
Understanding the full scope of how transgender hormone therapy will affect your body as it changes is important for all patients who are considering this option. Certain effects of transgender hormone therapy are long-term changes and, generally, are not reversible. These may entail:
Transitioning to your true gender is certainly a thrilling, life-changing decision. For more on the effects of transgender hormone therapy, contact HEALOR™ in Las Vegas, NV and schedule your visit today. Double board-certified physician Dr. Raj Singh and our team have advanced expertise in guiding trans men and trans women through the transition process and are excited to help you achieve your treatment goals.

How is HRT For Trans Men Different from Trans Women?
Choosing to undergo a female to male transition or a male to female transition is an important decision for many of our patients. If you’re considering transgender hormone therapy, experienced double board-certified physician Dr. Raj Singh at HEALOR™ works with the LGBTQ community regularly to help them start their gender affirmation journey.
Gender dysphoria is a sense that someone’s identity doesn’t match their biological sex, which can lead to depression and anxiety. Many patients with gender dysphoria choose to transition to their preferred gender. During a consultation in Las Vegas, NV, men and women can learn if they’re candidates for transgender hormone therapy, a type of hormone replacement therapy (HRT). We can discuss estrogen pills or testosterone injections with patients interested in HRT.
Transgender hormone replacement therapy involves administering different hormones to help Las Vegas patients acquire the look of their preferred gender. At HEALOR™, Dr. Singh offers a safe space for patients receiving this therapy. Treatment varies from patient to patient. A transgender man may need testosterone, and a transgender female may need estrogen. We administer hormones in pill form, with topical creams, or by injection.
Dr. Singh is experienced with hormone replacement therapy and can determine the proper method and dosage for each patient. Results will occur over time. He usually starts with low dosages to make sure that treatment is as safe as possible. Many patients experience changes in their appearance in six months to a year after starting transgender hormone therapy.
Each patient may experience different side effects of transgender hormone therapy. Some common physical effects during feminizing hormone therapy include:
Some symptoms of masculinizing hormone therapy can include:
During your visit to HEALOR™, Dr. Singh can discuss symptoms from hormone replacement therapy with his patients, so they know what to expect.
When you’re considering transgender hormone therapy in Las Vegas, Dr. Singh can answer all of your questions before therapy begins. Some of the most frequently asked questions about hormone replacement therapy include:
Yes, we do require a letter of statement from a psychiatrist or counselor before you start HRT.
Patients on testosterone can expect cessation of menstrual periods in about six months.
Patients can experience male pattern baldness, an increase in red blood cell production, which increases your risk of stroke or heart disease, and elevated cholesterol and liver enzymes.
Patients can experience elevated lipid levels such as triglycerides, an increased risk of developing breast cancer, and an increased chance of developing blood clots.
At HEALOR™, we offer compassionate and confidential care for the LGBTQ community. Dr. Raj Singh understands HRT for transgender men and women and can safely help with this transition. When you want to learn more about transgender hormone therapy, call our Las Vegas, NV office to schedule a consultation to learn about the benefits of HRT.