Hormone Disorders and Their Impact on Transgender Hormone Therapy
Hormone disorders can impact transgender hormone therapy by affecting the body’s ability to absorb, metabolize, and utilize the hormones administered. Hormone disorders can occur when the body produces too much or too little of certain hormones or when there is an imbalance in the levels of hormones in the body. This informative article will discuss thyroid disorders, polycystic ovary syndrome (PCOS), adrenal disorders and hypogonadism and their effect on transgender hormone therapy.
PCOS and Transgender Hormone Therapy
Polycystic ovary syndrome is associated with increased ovarian production of androgens such as testosterone, typically between ages 15-45. There is also an increased rate of anxiety and depression with PCOS.
Masculinizing hormone therapy is a medical treatment used to induce masculinization in transgender men or gender non-conforming individuals who wish to achieve a more masculine appearance or gender identity. This typically involves testosterone therapy, which can help promote the development of male characteristics such as cessation of the menstrual cycle, facial and body hair growth, a deeper voice, and increased muscle mass.
Masculinizing hormone therapy typically will begin producing changes in your body within weeks to months. In individuals with PCOS, the timeline of these changes may differ from those without PCOS.
Although this is an area of limited research, recent data has shown that starting testosterone therapy does not exacerbate PCOS symptoms and may help improve some of the metabolic problems associated with PCOS.
Thyroid disorders and Transgender Hormone Therapy
Thyroid disorders are conditions that affect the function of the thyroid gland, a butterfly-shaped gland located in the neck that produces hormones that regulate metabolism and other bodily functions. The two most common thyroid disorders are hypothyroidism and hyperthyroidism.
Hypothyroidism occurs when the thyroid gland does not produce enough thyroid hormone, slowing the body’s metabolic processes. This can cause fatigue, weight gain, constipation, dry skin, and cold intolerance.
Hyperthyroidism, on the other hand, occurs when the thyroid gland produces too much thyroid hormone, accelerating the body’s metabolic processes. This can cause symptoms such as weight loss, rapid heartbeat, anxiety, sweating, and tremors.
Transgender individuals on feminizing hormone therapy
Transgender HRT with estrogen can have a higher incidence of hypothyroidism than the general population. Estrogen therapy is associated with increased production of thyroid-binding globulins (TBG), which bind to thyroxine or T4 and prevent conversion to the active or free form of thyroid hormones called Tri-Iodothyronine or T3 hormone. The net result is the thyroid produces more T4 to compensate for this effect. This can overstress a weak thyroid gland and cause long-term hypothyroidism issues.
Individuals on estrogen-feminizing therapy can have typical symptoms of hypothyroidism. However, thyroid-binding globulin levels are not routinely checked, and thyroid hormones can remain normal. This often results in an undiagnosed or undertreated thyroid problem and may exacerbate underlying depression and chronic fatigue in transgender patients. Transgender individuals on estrogen therapy with symptoms of hypothyroidism should request their doctor to order thyroid-binding globulin (TBG) and free thyroid hormone (FT4, FT3) levels to diagnose this condition.
Transgender Individuals on Masculinizing hormone therapy
Hypothyroidism is also associated with high total testosterone and low free Testosterone levels, possibly due to increased production of sex hormone binding globulin ( SHBG ) by the liver. This results in too much bound or inactive form of testosterone. Transgender men with untreated hypothyroidism can require higher doses of testosterone to achieve the desired results, which may result in accelerated aromatization to estrogen and a higher percentage conversion to dihydrotestosterone (DHT) which can lead to adverse effects.
Just like hypothyroidism, individuals with hyperthyroidism can have high total testosterone and low free Testosterone levels, (area of debate) associated with significant elevations of the mean total testosterone and sex hormone-binding globulin (SHBG) levels and significant reduction of free Testosterone.
In addition, elevated estradiol levels and enlarged breasts (gynecomastia) are common in hyperthyroidism, which can negatively impact a transgender person’s masculinization journey.
Adrenal disorders and Transgender Hormone Therapy
The adrenal glands are two small, triangular-shaped glands located on top of the kidneys. They play an important role in regulating various bodily functions, including metabolism, blood pressure, immune system function, and the body’s response to stress.
Disorders of the adrenal glands can occur when these glands produce too much or too little of certain hormones, leading to a wide range of symptoms and health problems. Some common adrenal disorders include:
Addison’s disease:
A condition in which the adrenal glands do not produce enough cortisol and aldosterone, leading to symptoms such as fatigue, weight loss, low blood pressure, and electrolyte imbalances.
Antiphospholipid antibody syndrome (APL) is a potential cause of Addison’s disease. APL is a condition where individuals have a higher risk of developing blood clots. This can be particularly concerning for transgender women who are undergoing estrogen therapy, as they may be at an increased risk for blood clots and other complications.
Adrenal glands, also produce prohormones like dehydroepiandrosterone (DHEA) and DHEA sulfate. People with Addison’s disease may experience low libido and chronic fatigue due to the lack of these hormones. While DHEA supplementation can help alleviate these symptoms and improve overall well-being, it can also complicate hormone therapy for transgender patients with Addison’s disease. This is because DHEA can be converted into testosterone and estrogen, which can interfere with hormone therapy management.
Congenital adrenal hyperplasia (CAH):
is a genetic disorder that affects the production of adrenal hormones, leading to symptoms such as abnormal genitalia, infertility, and electrolyte imbalances. In some cases, CAH can also affect the production of sex hormones, leading to variations in gender identity and sexual development. Individuals with CAH may experience differences in gender identity and sexual orientation, as well as physical changes such as ambiguous genitalia or early onset of puberty.
Some individuals with CAH may identify as transgender or may seek gender-affirming treatments such as hormone therapy or surgery. For transgender individuals with CAH, hormone therapy can be complicated due to the underlying hormone imbalances associated with the condition. Testosterone therapy for transgender men with CAH may increase the production of androgens, which can exacerbate symptoms of CAH such as acne and excessive hair growth. Similarly, estrogen therapy for transgender women with CAH may exacerbate symptoms of CAH such as menstrual irregularities and electrolyte imbalances.
Hypogonadism and Transgender Hormone therapy
Hypogonadism is a condition in which the body does not produce enough of the sex hormones testosterone and/or estrogen. For transgender individuals undergoing hormone replacement therapy (HRT) as part of their gender transition, hypogonadism may be a concern. This condition requires lifelong treatment with either testosterone or estrogen, depending on the individual’s gender identity. Due to the lack of hormone production by their native glands, higher doses of hormones may be necessary to achieve the desired physical changes. Pellets are a form of hormone therapy that offers a unique advantage over other methods such as injections, gels, or oral medication. They provide long-term hormone therapy, making them an attractive option for those with hypogonadism.
Gender euphoria in PCOS
The relationship between PCOS and gender euphoria is complex and multifaceted, and the experience of gender identity and euphoria is unique to each individual. It is important to understand that not all individuals with PCOS identify as transgender or experience gender euphoria. However, for some transgender men with PCOS, the physical changes that come with the condition may align with their gender identity and be affirming.
As this is a relatively unexplored topic, I have made every effort to ensure the accuracy of the information presented. However, I welcome any feedback or differing opinions you may have. Please feel free to share your own experiences and thoughts by leaving a comment below.
Thanks for Reading!
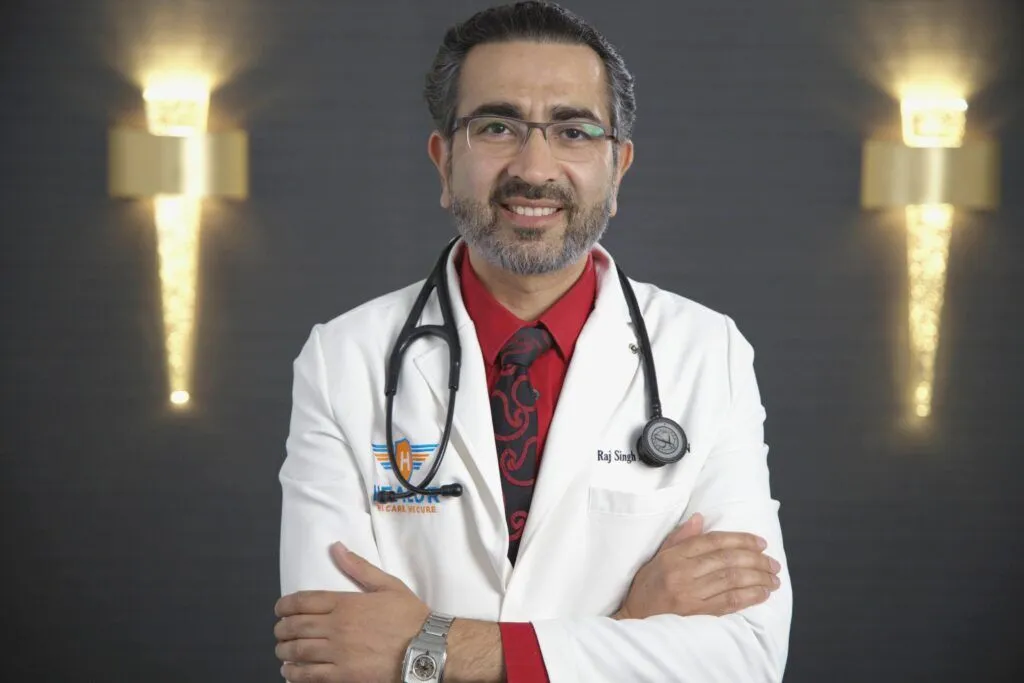
Raj Singh MD, FACP, FASN